Post-Op Sensitivity
Postoperative tooth sensitivity with composite restorations relentlessly continues to be a common, yet unpredictable, problem in dentistry. Caries, unless extensive, is generally considered to be a “silent” disease, making post-op sensitivity even more unforgiving when the extreme sensitivity occurs on teeth that were not sensitive before the restorations were placed. It is important to note that these undesirable outcomes far out way the more extensive & expensive treatment resulting from postponing or avoiding necessary dental care.
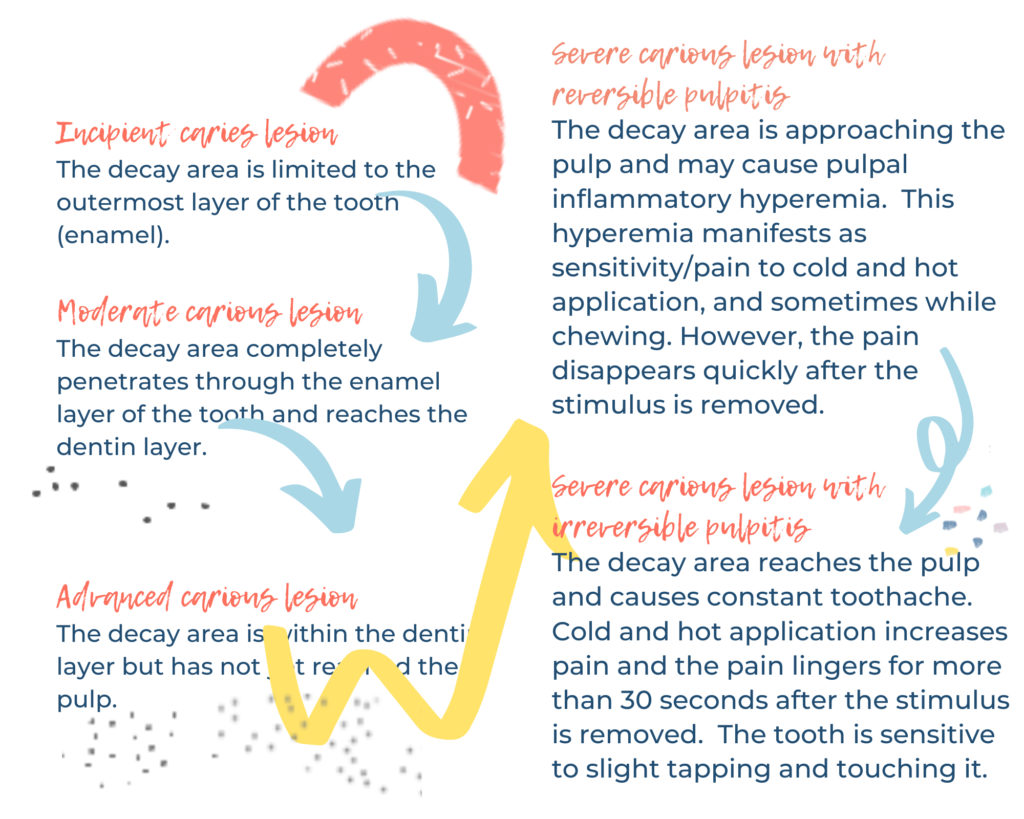
Decay and existing fillings can act as an insulation over the nerve and dentin. Wiping this insulation away during the restorative process, while introducing mechanical (the “drill” ) & chemical (bonding agents) trauma to the nerve tissue, can result in the post-op hypersensitivity. Post-op discomfort is usually attributed to the nerve’s response to these different forms of trauma introduced during treatment. When a tooth is treated, there is potential of irritating the nerve inside the tooth. The nerve may respond by becoming inflamed, which in turn can lead to sensitivity to cold and chewing. While the tooth heals, you should notice the sensitivity getting less frequent and less severe. This healing process may take days to weeks, and in some cases months.
We tell our patients that any time a tooth is drilled on, there is potential for some post operative sensitivity. The more work the tooth requires, or the deeper the decay, usually results in more sensitivity. The range of sensitivity is different for every patient. If the temperature sensitivity persists for a few weeks, it may be normal for you, but should slowly shows signs of improvement. In some cases, where there was more extensive decay, post operative sensitivity is likelihood and the health of the tooth may need to be monitored over time.
Understanding Tooth Anatomy:
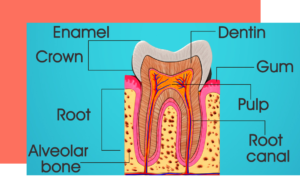
Enamel is the outermost layer and is a much tougher and less porous structure than dentin. Enamel, the hardest tissue in the body, covers the dentin and forms the outermost layer of the crown. It enables the tooth to withstand the pressure of chewing and protects it from harmful bacteria and changes in temperature from hot and cold foods.
Dentin lies below the enamel, and contains thousands of microscopic channels that have nerve endings. These channels are filled with fluid and conduct impulses or sensations to the pulp. Hot, cold, and sweet foods can cause the fluid to move and, as result, trigger a response that typically can manifest as a twinge of discomfort or short, sharp pain.
Some reasons a tooth may become sensitive after a filling or crown:
1. High Bite
It is common for the bite that to be slightly off or “high” after a filling is placed. In this case, it may not seem like a big issue at first, but the tooth can (and will) become sore and very sensitive to chewing after a few days. Do not hesitate in these cases to return to the office to have this high spot evaluated and adjusted. It is a very quick and easy process. This requires a quick chairside adjustment, thus relieving the bite. Often this is all that is necessary to make the tooth comfortable.
2. Reversible Pulpitis
Pulpitis is defined as inflammation of the pulp. And in the case of reversible pulpitis, it is expected that this inflammation will resolve and heal over time. Because the pulp is in a confined space (in the middle of your tooth) it really doesn’t have anywhere to expand and thus it causes the tooth to feel sore as the tissue expands against the wall of the canals. Most of the time the pulp will settle down within a couple of days or weeks, much like a bump or a bruise does. This will manifest as pain on stimulation with hot/cold, and pain does NOT persist.
3. Irreversible Pulpitis
Often times, when there is a deep cavity, one that is near the pulp, the pulp becomes irritated so much that it can not heal/resolve and the nerve tissue starts to die. With a deep cavity, microscopic bacteria may already be affecting and/or infecting the pulp. We oftentimes do our best to insulate the pulp with a base under the filling. However, once a pulp starts to die, the only treatment we can do to save the tooth is a root canal therapy. The symptoms associated with this diagnosis can be intense or throbbing pain, pain that persists after hot/cold stimulus is removed, pain that wakes you up during your sleep, or spontaneous pain.
Things you can do to reduce post-op sensitivity:
Any time you have sensitivity or questions about your symptoms, call or email us!! Communication is key! Based on your symptoms and the information you provide, we can provide recommendations that may help. Some recommendations we provide our patients are as follows:
-
Use of Anti-inflammatory medication:
We generally advise use of 400mg of Ibuprofen every 8 hours for a few days post-op. This can also be combined with Tylenol 500 for improved pain management. Tylenol can be taken every 6 hours. It is also important to take this with food.
-
Sensodyne use:
After brushing with Sensodyne, flossing, and rinsing with fluoridated rinse, you can take a small amount of Sensodyne on a Q-tip and place it along the gum long on the affected tooth. This should progressively help alleviate sensitivity.
-
Soft & Temperate Diet:
Hard &/or sticky foods can put the tooth under additional stress, exacerbating the inflamed pulp, resulting in pain/sensitivity. You can also try to avoid chewing directly on the filled tooth for the first days. As a general rule, take it easy on the affected side ie nothing too hard, nothing too hot or cold.
-
Good Oral Hygiene:
Continue brushing, flossing, and rinsing as usual, despite any discomfort or soreness. This will assure proper gum healing post-op and eliminate this as a source of discomfort. Rinsing with warm water and salt will also speed up the gum healing.